As we know, communities are vast ecosystems, interconnected strands of individuals, families, and institutions, all interwoven through shared experiences and societal structures. Within this web, the struggles of one ripple outward, impacting the collective wellbeing. Nowhere is this truer than in the realm of addiction.
Substance use disorders (SUDs) weave a complex tapestry of personal hardships, economic burdens, and social decay. Addressing them requires a systemic approach, one that understands communities as interconnected and adopts a standard of care that prioritizes evidence-based, personalized treatment for all. This is where the ASAM Criteria, developed by the American Society of Addiction Medicine, rises to prominence.
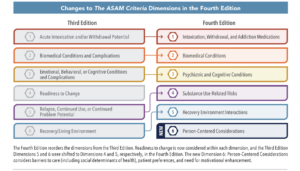
These comprehensive guidelines assess six key dimensions – acute intoxication, biomedical conditions, emotional and behavioral health, readiness to change, risk of relapse, and recovery environment – to match individuals with the most appropriate level of care. In essence, the ASAM Criteria act as a bridge, connecting the specific needs of individuals within a community to a spectrum of accessible, evidence-based interventions.
Why is this crucial? Consider the current state of SUD treatment. Fragmentation, inconsistency, and systemic inequities plague the system. Individuals often navigate a labyrinth of options, lacking a clear roadmap to the care they desperately need. This disconnect between need and resources has devastating consequences. Undiagnosed and untreated SUDs fester, eroding individual lives and impacting the fabric of a community. Crime rates rise, families shatter, and societal costs balloon.
Read more here: Kindness, Equity, and the Mental Health Crisis: The View from this Nurse’s Window
The ASAM Criteria offer a paradigm shift. By establishing a unified, data-driven framework for assessing and addressing SUDs, they provide a compass for both individuals and community systems. Clinicians can utilize the framework to develop personalized treatment plans, while policymakers and healthcare providers can leverage it to allocate resources efficiently and equitably.
This standardization removes guesswork and ensures that every individual, regardless of zip code or socioeconomic background, consistently receives the level of care they need to heal and thrive.
Here’s how this translates into tangible benefits for communities:
- Improved Health Outcomes: By matching individuals with the right level of care, the ASAM Criteria can lead to better adherence to treatment plans, higher success rates in overcoming SUDs, and a reduction in associated health complications.
- Enhanced Safety and Security: Reduced rates of addiction correlate with lower crime rates, fewer accidents, and stronger social cohesion. Investing in treatment based on the ASAM framework translates to safer and more vibrant communities.
- Greater Economic Vitality: The costs of untreated SUDs are staggering, impacting healthcare systems, lost productivity, and criminal justice expenses. Effective treatment, as guided by the ASAM Criteria, can significantly reduce these burdens and redirect resources towards community growth.
- Empowered Individuals and Families: When individuals can access appropriate treatment and build sustainable recovery, they re-enter the community as active, contributing members. This strengthens the social fabric and empowers families to thrive.
The transition from the Pennsylvania Client Placement Criteria (PCPC) to the American Society of Addiction Medicine (ASAM) Criteria in Pennsylvania for substance use disorder (SUD) treatment is reportedly complete as of July 1, 2018.
Here’s a summary of the current status:
- ASAM is now the standard tool for level of care (LOC) placement for adults seeking SUD treatment in Pennsylvania.
- The transition aimed to achieve several objectives, including:
- Individualized treatment: Move from program-defined to patient-centered care.
- Nationally recognized standard: Facilitate consistency across providers and payers.
- Financial benefits: Address Medicaid managed care requirements and access federal funding.
- Improved data collection: Align with the new DDAP treatment data system.
- Training and resources: Extensive training for clinicians and providers took place before and after the transition. Additional resources are available through the Pennsylvania Department of Drug and Alcohol Programs (DDAP) website.
- Ongoing monitoring: DDAP continues to monitor the implementation of ASAM and provide support to stakeholders.
Viewing communities as interconnected systems and adopting the ASAM Criteria as the standard of care for SUD treatment is not just a clinical or policy decision; it’s a social imperative. It’s about recognizing that the well-being of each individual is inextricably linked to the collective health of the community. By bridging the gap between needs and resources, the ASAM Criteria can guide us towards a future where addiction no longer dictates the narrative of our communities, but serves as a challenge we overcome together, paving the way for a stronger, healthier, and more equitable future for all.
If you want to learn more about ASAM in Pennsylvania, you can visit the following resources:
- DDAP ASAM Transition page: https://www.ddap.pa.gov/Professionals/Pages/ASAM-Transition.aspx
- FAQ Regarding Transition to ASAM: https://www.ddap.pa.gov/Professionals/Pages/ASAM-Transition.aspx
- Guidance for Application of ASAM in Pennsylvania’s SUD System of Care: https://www.ddap.pa.gov/Professionals/Pages/ASAM-Transition.aspx
- To learn more about ASAM, visit them at ASAM.org.